Imagine the throbbing pain of a toothache – it’s a signal that something is amiss with your dental health. Root canal therapy, although a much-feared dental procedure, is a saving grace for such distressing situations. It’s essential to understand what a root canal is and why it might be necessary for restoring your oral health.
Understanding Root Canal Treatment
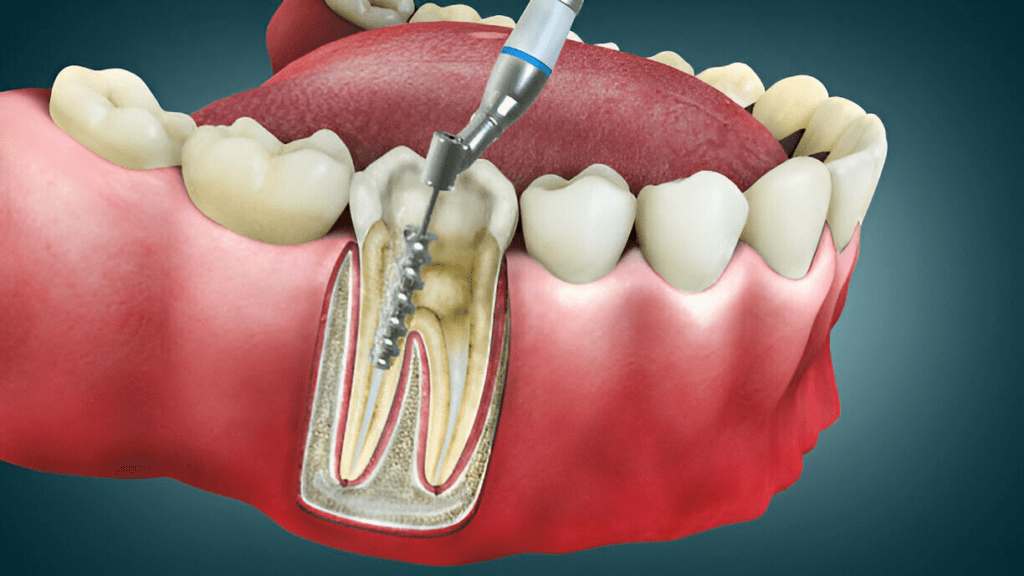
Root canal treatment, often simply referred to as a root canal, is a dental procedure that is essential in saving and repairing a tooth that is badly decayed or infected. This endodontic treatment involves removing the infected or inflamed pulp from within the tooth’s root canals, cleaning and disinfecting the area, and then filling and sealing it with a biocompatible material. The natural tooth is thus preserved, which benefits not only an individual’s oral health but also their overall well-being.
The root canal procedure typically takes place over one or more visits to the dentist or endodontist, a dental specialist focusing on such treatments. Factors that affect the duration include the severity of the infection, the number of root canals in the tooth, the type of tooth affected, and whether or not any complications arise.
After the infected or damaged pulp is removed, the dentist may insert a temporary filling to protect the tooth until a permanent filling or dental crown can be placed. This multi-step process is vital in preventing tooth extraction and maintaining as much of the natural tooth structure as possible. Proper dental care following the procedure can lead to high success rates and a healthy, functioning tooth for years to come.
What is a root canal?
A root canal is a common dental procedure designed to address problems in the soft tissues, or dental pulp, inside a tooth. This pulp contains blood vessels, connective tissue, and nerves which can become infected or inflamed due to deep decay, a chip or crack in the tooth, or repeated dental treatment.
The term “root canal” not only describes the procedure itself but also the natural cavities within the tooth where this dental pulp resides. During the root canal procedure, the dentist removes the affected pulp, and meticulously cleans and shapes the inner chamber of the tooth before filling it with a permanent material. This process eliminates bacteria and protects the tooth from future microbial invasion. The final restoration usually includes a dental filling or a crown that restores the tooth to its full function and appearance.
Why is root canal treatment necessary?
Root canal treatment is necessary when the dental pulp within a tooth becomes infected or inflamed. This condition can result in tooth pain and may lead to an abscess if left untreated. Causes of such an infection include deep tooth decay, repeated dental procedures on the same tooth, faulty crowns, or a crack or chip in the tooth. In some cases, trauma to a tooth may damage the pulp even if there are no visible cracks or chips.
Without treatment, the infection can worsen, leading to more severe pain and swelling. In extreme cases, the infection can spread beyond the tooth, affecting other oral structures, and may have systemic implications for overall health. A root canal is thus a critical procedure to eliminate the infected part of the tooth, relieve pain, and save the natural tooth from extraction. By preserving the natural tooth structure, patients maintain their normal biting force and sensation, and natural appearance, and prevent other teeth from drifting out of alignment.
Step 1: Preliminary Examination
Before a dentist can perform a root canal, a thorough preliminary examination is crucial. This initial evaluation ensures accurate treatment planning and helps determine the best course of action for the patient. The dentist will typically start with a review of the patient’s dental and medical history, followed by a clinical assessment of the tooth in question.
Diagnosis of an infected tooth
The diagnosis begins with a visual inspection, where the dentist looks for signs of tooth decay, damage, or infection. This may involve probing the tooth and surrounding gums to check for sensitivity or swelling. Dental x-rays or, in some cases, 3D imaging such as cone-beam computed tomography (CBCT), are taken to view the internal structures of the tooth and the bone around it. These images help in identifying the presence of an infection, abscesses, or the extent of the damage not visible to the naked eye.
Evaluation of the severity of the infection
Evaluating how far the infection has progressed is critical. The dentist may assess factors such as the level of pain, swelling, and the presence of pus. Moreover, the X-rays play a key role in showing if the infection has spread into the surrounding bone or if there is a visible dark spot at the tip of the root, which indicates an abscess.
Assessing the suitability for root canal treatment
Once the infection is confirmed and evaluated, the dentist must determine if the tooth is a good candidate for root canal treatment. This decision is based on numerous factors, including the tooth’s structure, the integrity of the supporting bone, and the patient’s overall health and dental care routine. If there is too much damage or the structure of the tooth is compromised, alternative treatments like tooth extraction might be considered.
Preliminary Examination for Root Canal Treatment
| Examination Step | Details |
|---|---|
| Visual Inspection | Check for visible signs of decay or damage |
| Palpation and Percussion | Feel for swelling, test for sensitivity or discomfort |
| Dental Imaging | X-rays or CBCT to view the extent of infection and damage |
| Symptom Evaluation | Review symptoms such as pain or swelling to assess infection level |
| Structural Assessment | Determine the remaining tooth’s integrity and bone support |
| Treatment Suitability | Decide if root canal is viable or if other treatments are needed |
By following this systematic process, the dentist can provide an accurate diagnosis and tailor the treatment plan to each individual patient’s needs, thereby ensuring the best possible outcome for the tooth in question.
Step 2: Administering Anesthesia
Administering anesthesia is a critical step in the root canal procedure, which precedes the actual treatment of the tooth. This step is essential to ensure the patient feels no pain during the process, making the experience as comfortable as possible.
Local anesthesia for pain relief
When the time comes to commence the root canal therapy, the first thing a dentist does is numb the area around the infected tooth. Local anesthesia is employed to block pain signals from the affected tooth and surrounding tissues. The anesthetic is injected into the gum or inner cheek, and within a few minutes, the area becomes numb, providing relief from the often intense tooth pain associated with an infected pulp.
The type and amount of anesthesia used can vary depending on the complexity of the case and the patient’s sensitivity to pain. The goal is to effectively manage pain and minimize discomfort so that neither the patient nor the dentist is hindered by potential movements or reactions during the procedure. Before proceeding, the dentist will usually wait a few minutes to ensure the area is fully numb. Throughout the treatment, the patient should expect to feel some pressure but no pain.
Different types of anesthesia used during root canal treatment
Root canal treatments are typically associated with local anesthesia; however, there are instances where different anesthesia or sedation methods might be considered. Here’s a breakdown of the commonly used options:
| Type of Anesthesia | Description |
|---|---|
| Local Anesthetic | Local agents like lidocaine are injected near the tooth to numb a specific area. |
| Nitrous Oxide (Laughing Gas) | Used for mild sedation, helps reduce anxiety and discomfort without putting the patient to sleep. |
| Oral Conscious Sedation | Oral medications are prescribed before the procedure to help relax the patient during treatment. |
| Intravenous (IV) Sedation | Administered directly into the bloodstream; used in more anxious patients and controlled by a professional. |
| General Anesthesia | Rarely used in root canal treatment, it makes the patient completely unconscious. |
The choice of sedation is based on the patient’s anxiety level, the complexity of the procedure, and the dentist’s or endodontist’s recommendation. Local anesthesia is most common, but for patients with dental phobias or special needs, sedation might be an additional option to ensure their comfort and cooperation during the process.
By carefully selecting the appropriate type and application of anesthesia, dentists ensure that the root canal procedure is pain-free and anxiety-free for their patients. It sets the stage for a smooth dental experience, leading to the restoration of the natural tooth while maintaining the patient’s comfort and well-being.
Step 3: Accessing the Infected Tooth
Once the area is sufficiently numb from the anesthesia, the dentist moves on to the third step of the root canal process — accessing the infected tooth. This step is pivotal as it sets the pace for the rest of the procedure and involves precision to avoid any further damage to the tooth.

Creating an opening in the tooth
To reach the diseased or damaged pulp, the dentist needs to create an opening in the top part of the tooth. Using special dental instruments, such as drills and files, a careful and methodical process begins to access the inner chamber of the tooth. Typically, this is done on the biting surface of the tooth for molars and premolars or from behind the tooth in the case of front teeth.
The opening needs to be large enough to clean the canals within the tooth but small enough to maintain as much tooth structure as possible. The goal is to be precise, ensuring the natural tooth is prepared for a temporary filling and, eventually, a dental crown to provide strength and protection after the root canal treatment.
Removing decayed and damaged tooth structure
Once the dentist has access to the inner chamber, the next crucial step is to remove the decayed and damaged tooth structure to prevent the spread of infection. Here, the dentist uses fine dental instruments to meticulously remove not only the infected pulp but also any debris and bacteria present within the tooth’s canals.
The process involves:
| Step | Description |
|---|---|
| Cleaning the root canals | Special instruments and antibacterial solutions are used to clean out the entire canal system thoroughly. |
| Shaping the canals | The canals are shaped with tiny files to allow for proper filling and sealing in subsequent steps. |
| Decontaminating the tooth interior | The cleaned and shaped canals are flushed with antiseptic and antibacterial medications to disinfect thoroughly. |
The focus during this part of the treatment is not only to remove the infected part but also to preserve as much of the healthy structure of the tooth as possible. This ensures that the natural tooth is as functional as possible after the completion of the root canal therapy.
By approaching the third step of the procedure with precision and care, the dentist ensures the successful removal of the infected pulp, setting a strong foundation for the healing process and the restoration of the natural tooth to its full form and function.
Step 4: Cleaning and Shaping the Root Canals
Root canal therapy demands scrupulous cleaning to ensure the removal of infected tissue and bacteria. It is a cornerstone in safeguarding against future infections and an essential stage before sealing the tooth.
Removing Infected Pulp and Bacteria
The primary goal at this stage of the dental procedure is the thorough eradication of bacteria and the infected pulp from within the root canals. The dental pulp contains nerves, connective tissue, and blood vessels that can harbour bacteria when an infection settles in. By meticulously clearing out the pulp and bacterial contaminants, endodontic treatment aims to alleviate tooth pain and restore healthy conditions within the tooth.
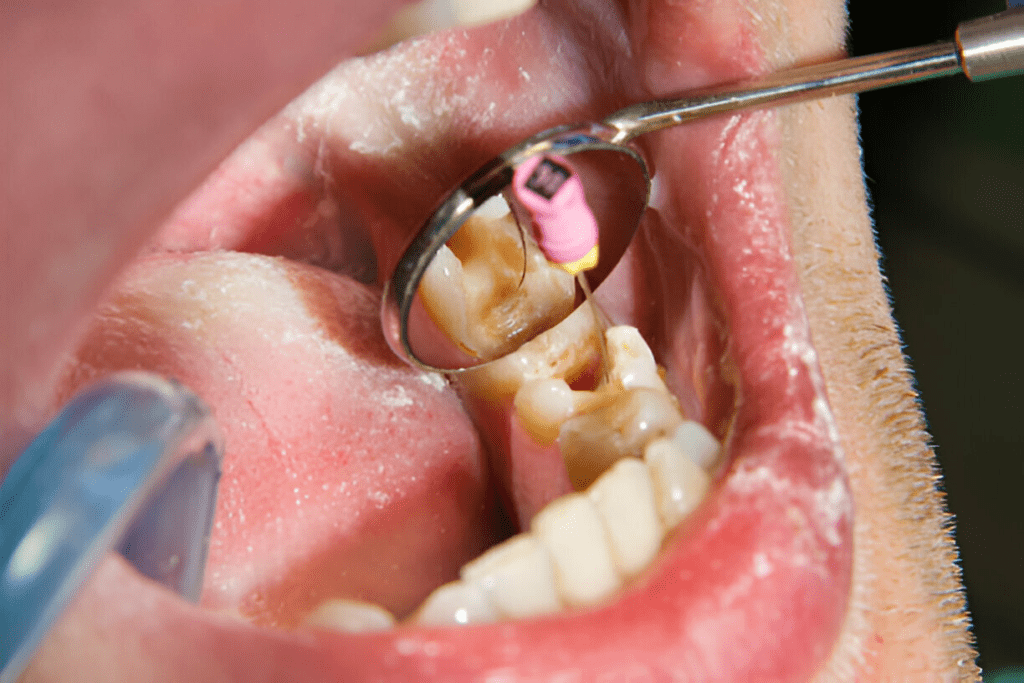
Utilizing Specialized Instruments for Thorough Cleaning
Dentists employ a variety of precision instruments to clean the root canals meticulously. These instruments include small files that come in various sizes to accommodate the differing canal sizes and shapes within a single tooth or between different types of teeth, such as molars and canine teeth.
| Instrument | Purpose |
|---|---|
| Endodontic Files | To remove the infected pulp and shape the canals. |
| Irrigants | To flush out debris and kill bacteria within the canal. |
This combination of specialized instruments and antibacterial solutions ensures that even the tiniest spaces within the canal system are reached and cleansed.
Shaping the Root Canals for Optimal Filling
After the infected material is removed, the next critical step is to reshape the canals so that they can snugly accommodate a biocompatible material, usually gutta-percha, during the filling process. This shaping allows for a tight seal, which is crucial in preventing reinfection.
The reshaping process typically involves:
- Enlarging the canals to make sufficient room for the filling material.
- Smoothing the canal walls to foster a firm and even seal.
- Creating a conical form within the canal for optimal filling distribution.
The meticulous shaping and cleaning process establishes a path for the successful placement of a temporary filling, which will later be replaced by a permanent filling or dental crown to restore full functionality and aesthetics to the natural tooth.
Step 5: Temporary Filling
Once the root canals have been meticulously cleaned and shaped, the next phase in the root canal treatment involves placing a temporary filling. This stage is crucial to protect the delicate work done so far and to ensure that the canals are securely sealed off from any potential bacterial invasion between appointments.
The temporary filling is an interim solution that safeguards the tooth until the permanent filling or dental crown is ready to be installed. It’s a critical barrier against contamination and helps to maintain the integrity of the dental work while the tooth heals.
This filling also provides relief by alleviating tooth pain and sensitivity that can occur after the procedure. By sealing the canals, it reduces the potential for further infection and allows the natural tooth to begin the recovery process before the final restoration.
Protecting the root canals between appointments
The root canal system is intricate, consisting of numerous small passages that extend from the crown to the tip of the root. Following the removal of the infected pulp, these pathways remain highly susceptible to new infections. Thus, protectively sealing them with a temporary filling is paramount.
Between appointments, patients must take special care not to dislodge this temporary filling. It is generally recommended to avoid chewing on the affected side of the mouth and to maintain good oral hygiene. This care is essential in upholding the success rates of the root canal therapy by ensuring no new contaminants compromise the treated area.
Materials used for temporary fillings
Temporary fillings are designed to be durable enough to withstand the pressures of daily use but also removable such that they can be taken out easily by the dentist when it’s time to place a permanent filling. Common materials used include:
| Material | Characteristics |
|---|---|
| Eugenol-based cements | Has soothing properties and eases discomfort |
| Zinc oxide eugenol cement | Offers good seal and easy removal |
| Glass ionomer cement | Releases fluoride which can help protect the tooth |
| Composite resin | Stronger and may be used when a longer-lasting temporary is needed |
These materials are chosen for their biocompatible nature and their ability to be easily manipulated and formed to the precise shape of the cleaned canals. The temporary filling remains in place usually for a few days to a couple of weeks until the patient returns for the final phase of the root canal procedure, which is the placement of a permanent filling or, more commonly, a dental crown.
The selection of the specific material often depends on the dentist’s preference, the length of time the temporary filling needs to last, and the patient’s individual circumstances, such as whether they have any allergies or sensitivities to particular components.
Step 6: Recovery and Waiting Period
After the temporary filling is set, the recovery and waiting period begins. This critical phase allows the natural tooth to heal and settle after the invasive procedure of a root canal. It often spans from a few days to a couple of weeks and is integral to the success of the root canal therapy.
During this time, patients might experience some inflammation as the body reacts to the recent dental work. Such a response is natural—the oral soft tissues and surrounding connective tissue may need time to recover from the treatment and start the healing process.
The dental care provider will typically schedule a follow-up appointment to complete the procedure with a permanent filling or dental crown. This period between appointments is crucial because it offers the dentist insight into how the tooth and surrounding tissues are healing and ensures that no further infection is present.
Healing time can vary based on the severity of the infection, the complexity of the root canal, and the individual patient’s response to treatment. Patients must follow their dentist’s specific aftercare instructions to facilitate a smooth recovery process and return for the final restoration as scheduled.
The Importance of Allowing Time for the Tooth to Heal
Healing is a significant step in the root canal process, one that should not be rushed. Allowing adequate time for the tooth to heal helps ensure that any residual bacteria are dealt with and that the tooth’s integrity is reinstated.
During healing, the tooth is essentially recovering from the removal of the infected pulp, inflammation, and any other issues that might have arisen before or during the procedure. The repair of tiny nerves and blood vessels around the tooth begins, and the bone surrounding the root can start to heal and reattach firmly to the natural tooth.
Without this crucial rest period, patients run the risk of complications such as post-treatment infections or a breakdown of the temporary filling, possibly leading to the need for additional dental treatment or even tooth extraction.
Managing Discomfort During the Waiting Period
While the temporary filling reduces sensitivity and discomfort, some degree of pain or unease is to be expected during the post-root canal recovery. Here’s how patients can manage discomfort:
- Pain Management: Over-the-counter pain medications are effective for managing minor discomfort. Always use these medications as directed by your dentist or healthcare provider.
- Avoid Certain Foods: Keep away from hard, crunchy, or sticky foods that can dislodge the temporary filling or irritate the tooth.
- Maintain Oral Hygiene: Continue with gentle brushing and flossing around the treated area to keep it clean and aid in the healing process.
| Discomfort Management | Tips |
|---|---|
| Pain Medications | Over-the-counter options like ibuprofen |
| Eating Habits | Soft foods, avoid chewing on the treated side |
| Oral Hygiene | Gentle brushing, careful flossing |
It’s important to note that extreme or persisting pain should not be overlooked. If a patient experiences severe discomfort or signs of infection, they should contact their dental specialist without delay.
By taking these steps and monitoring any changes in their oral health, patients can effectively manage discomfort and contribute to creating an optimal environment for the permanent restoration of their tooth.
Step 7: Permanent Filling and Dental Crown

Removing the Temporary Filling
Once the natural tooth has sufficiently healed and the root canals are infection-free, your dentist will proceed to the next step: removing the temporary filling. This is usually done during a follow-up appointment. The removal process must be careful to avoid undue stress to the tooth, which has been given time to recover and begin the reattachment process to the surrounding bone.
Filling and Sealing the Root Canals with Biocompatible Material
After the temporary filling is removed, the cleaned root canals will be filled and sealed with a biocompatible material, most commonly gutta-percha. This rubber-like material is used because it’s compatible with the body and effectively fills the space where the dental pulp once was, preventing future infections.
| Canal Filling Steps | Materials & Functions |
|---|---|
| Cleaning | To ensure no debris or bacteria remain |
| Filling | Gutta-percha is inserted into the canals |
| Sealing | An adhesive cement seals the gutta-percha |
Placement of a Dental Crown to Restore the Tooth’s Strength and Function
The final stage involves restoring the tooth’s structural integrity with a dental crown. A crown is custom-made and could be made from different materials, such as porcelain or metal, depending on the location of the tooth and aesthetic considerations.
- Tooth Preparation: The tooth is shaped to properly fit the crown.
- Crown Fabrication: A mold of the tooth is made, and the crown is crafted to match the natural shape and color of your existing teeth.
- Crown Fitting: Once prepared, the crown is permanently cemented onto the tooth.
| Steps | Purpose & Outcome |
|---|---|
| Tooth Preparation | Ensures the crown will fit securely and comfortably over the natural tooth |
| Crown Fabrication | Tailors the crown to the exact specifications needed for the patient |
| Crown Fitting | Finalizes the process by securing and sealing the crown on the tooth |
The placement of a crown is a crucial component of both the function and long-term success of the root canal therapy. It not only reinforces the tooth but also provides a seamless appearance within the mouth. Post-procedure, most patients will regain full function, which includes biting and chewing without pain or discomfort.
It’s important for patients to maintain regular dental care and hygiene practices to protect the integrity of the dental crown and the health of the surrounding teeth. Regular dental check-ups are also vital in assessing the condition and longevity of the crown, ensuring that the treated tooth continues to function naturally and effectively.
Step 8: Aftercare and Follow-up
After the root canal therapy and placement of the dental crown, it is essential for patients to prioritize effective aftercare to ensure the best possible outcome for their dental health. Immediately following the procedure:
- Monitor for any signs of infection or discomfort. Some minor tenderness is normal, but severe pain or swelling should prompt a visit to the dentist.
- Follow your dentist’s instructions for care. This may include taking over-the-counter pain medications to alleviate discomfort.
- Contact your dentist if you experience any issues with the temporary filling or crown, such as it coming loose or falling out.
- Avoid chewing hard foods on the treated tooth until it is fully restored with a permanent crown to prevent any damage.
Effective Oral Hygiene Practices Post-Treatment
Maintaining good oral hygiene is critical after receiving root canal treatment. Here are some key practices patients should follow:
- Brush your teeth twice a day using a soft-bristled toothbrush and fluoride toothpaste to prevent cavities and gum disease.
- Floss daily to remove plaque and food particles between teeth, an area your toothbrush can’t reach.
- Use an antiseptic mouthwash if recommended by your dentist to reduce bacteria that can lead to infections.
- Be cautious with food. Avoid sticky and hard foods that can dislodge a temporary filling or crown.
- Do not smoke or use tobacco products, as they can inhibit healing and affect the success of the root canal treatment.
- Schedule regular dental check-ups for professional cleaning and to monitor the integrity of the root canal and crown.
| Oral Care Steps | Description |
|---|---|
| Brushing | Use a soft toothbrush; clean teeth gently but thoroughly. |
| Flossing | Should be done carefully; important for removing debris between teeth. |
| Rinsing | Antiseptic mouthwash might be recommended for antibacterial action. |
| Eating Habits | Chew gently, avoid hard and sticky foods. |
| Smoking | Should be entirely avoided for better healing and overall dental health. |
| Check-ups | Regularly visit your dentist for follow-ups and cleanings. |
These aftercare practices will help mitigate potential complications and will support the long-term success of root canal therapy, preserving your dental health and the function of your treated tooth.






