Denture stomatitis can be an uncomfortable and distressing condition, often affecting individuals who wear dentures. With a significant portion of the aging population relying on dentures, understanding this condition becomes increasingly vital.
This inflammation of the oral mucosa can result from various factors, including poor oral hygiene and ill-fitting dentures. Recognizing the symptoms and potential causes is essential for effective treatment and prevention.
In this article, we will explore the identification and treatment options for denture stomatitis, shed light on the importance of proper care, and discuss preventative measures to enhance oral health for denture wearers.
Understanding Denture Stomatitis
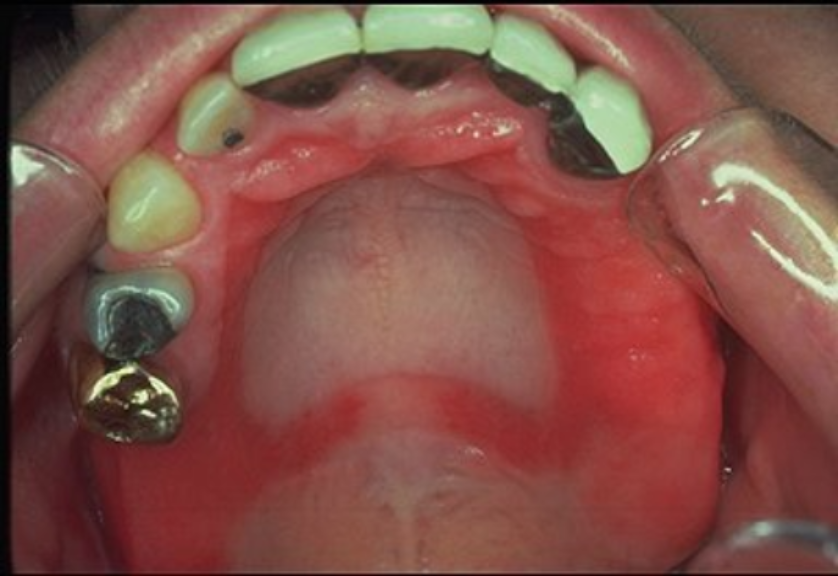
Denture stomatitis, often referred to as denture-related stomatitis, is a common condition experienced by denture wearers, characterized by inflammation of the oral mucosa beneath the denture. It predominantly affects the palatal mucosa in individuals with complete dentures. Symptoms of denture stomatitis include a sore mouth, redness, and sometimes yeast infections, such as those caused by Candida species.
The development of denture stomatitis is frequently associated with ill-fitting dentures, poor denture hygiene, and inadequate oral hygiene. These factors contribute to the buildup of microbial biofilms, leading to irritation and infection of the oral tissues. Nutritional deficiency and certain systemic conditions such as diabetes may also predispose individuals to this condition.
Dental professionals diagnose this condition by assessing clinical features and may recommend antifungal agents, particularly in the case of Candida-associated denture stomatitis. The management of denture stomatitis involves improving denture fit, enhancing oral and denture hygiene practices, and using medicated treatments as necessary.
The prevalence of denture stomatitis is notably higher in complete denture wearers, but it can affect those with partial dentures as well. It is essential for patients with denture stomatitis to follow their dental professional’s instructions for treatment to prevent complications, such as angular cheilitis.
Common Causes of Denture Stomatitis
Denture stomatitis is often attributed to several contributing factors, underlying conditions, and environmental influences. Recognizing these common causes is key for denture wearers to prevent and manage symptoms effectively. Three significant factors associated with the onset of denture stomatitis are poor oral hygiene, ill-fitting dentures, and Candida infections.
Poor Oral Hygiene
Maintaining good oral hygiene is crucial for anyone, but it becomes even more important for individuals wearing dentures. Inadequate cleaning of the oral cavity and dentures can lead to the accumulation of food particles, plaque, and the formation of microbial biofilms, which are contributors to denture-induced stomatitis. Practicing thorough oral hygiene and regular denture cleaning can significantly reduce the risk of developing this unwanted condition.
Ill-Fitting Dentures
Dentures that do not fit properly can create constant pressure or friction against the oral mucosa, leading to tissue irritation and inflammation. Over time, the oral cavity undergoes changes, and dentures may require adjustments or replacements to ensure a proper fit. Ill-fitting partial or complete dentures are a key factor that can disrupt the integrity of the oral tissues and may accelerate the development of stomatitis.
Candida Infections
Candida albicans, a type of yeast, is commonly found in the oral cavity but can overgrow and cause infections under certain conditions. Denture wearers are particularly susceptible to Candida infections, which can result in Candida-associated denture stomatitis. Antifungal treatment may be indicated to manage and resolve the infection, accompanied by a review of denture hygiene practices to prevent recurrence.
Recognizing Symptoms of Denture Stomatitis
Denture stomatitis, or denture-related stomatitis, is a common condition characterized by inflammation and irritation of the oral mucosa underneath a denture. This condition is typically seen in individuals who wear complete or partial dentures and can affect various parts of the oral cavity, but most often occurs beneath the upper denture, affecting the palatal mucosa. Recognizing the symptoms of denture stomatitis is critical for prompt and effective management of the condition, which can improve comfort and oral health for denture wearers.
Redness and Inflammation
One of the primary clinical features of denture stomatitis is redness in the area of the oral cavity that comes in contact with the dentures. The affected mucosa, particularly under the upper denture, may present with varying degrees of redness, often corresponding to the severity of the inflammation.
Dental professionals categorize this inflammation into different types, depending on the presentation of the erythema. In addition to redness, denture wearers may also notice swelling as part of the inflammatory response.
Soreness and Discomfort
Patients with denture stomatitis frequently report soreness and discomfort, especially when the dentures are in use. This discomfort could manifest as a constant mild irritation or progress to a more painful experience during chewing or when the dentures are touched.
Ill-fitting dentures tend to exacerbate such discomfort and may lead patients to seek corrective measures from dental professionals. It’s important for those experiencing these symptoms not to dismiss them as mere inconveniences, as continuing to wear offending dentures could lead to further oral complications.
Changes in Taste
In some cases, denture wearers with stomatitis may experience changes in taste or have an abnormal taste sensation. These changes can range from a metallic taste to a complete distortion or reduction of taste. Such sensory changes can be distressing and may negatively impact one’s enjoyment of food. While these changes in taste could be related to the infection itself, they can also be influenced by the presence of yeast infections, particularly Candida-associated denture stomatitis.
Recognizing the symptoms of denture stomatitis is essential for its management. By maintaining proper oral hygiene, ensuring a correct fit of the dentures, and regularly consulting with dental professionals, common issues such as sore mouth, discomfort, and changes in taste can be addressed before they lead to more serious complications. If you suspect you have symptoms of denture stomatitis, it is crucial to seek professional advice for an accurate diagnosis and appropriate treatment plan.
Diagnosis of Denture Stomatitis
Diagnosis of Denture Stomatitis involves a thorough clinical evaluation, often accompanied by various laboratory tests, to ascertain the presence and severity of the condition. Dental professionals play a pivotal role in diagnosing this common condition, which affects numerous denture wearers.
Clinical Evaluation
The clinical evaluation for Denture Stomatitis begins with a visual inspection of the oral cavity by dental professionals. They examine the palatal mucosa and the areas in contact with the dentures. Denture wearers typically present clinical features such as redness, swelling, and sometimes superficial ulcerations, particularly under the upper denture.
Patients with Denture Stomatitis may report symptoms like a sore mouth or discomfort. During the evaluation, the fit and cleanliness of the complete or partial dentures are assessed. Poor denture hygiene is a significant contributor to the development of denture stomatitis. Factors such as the duration of daily denture wear and overnight denture use are also considered during clinical examination since these habits can influence the prevalence of the condition.
Additionally, professionals will inquire about patients’ oral hygiene habits, the frequency of denture cleaning, and any instances of past yeast infections, which is essential to determining the best course of action for treatment.
Laboratory Tests
To confirm the diagnosis of Denture Stomatitis, particularly when yeast infections like Candida are suspected, laboratory tests may be necessary. These tests typically include:
- Swab cultures: Taken from the palatal mucosa beneath the denture to identify the presence of fungal organisms.
- Cytological smears: Assistance in assessing the type of infection and the presence of fungal hyphae.
- Biopsy: Rarely required, but may be performed to exclude other conditions if unusual clinical features are present.
These tests help differentiate Candida-associated denture stomatitis from other types of oral mucosa infections and conditions, such as angular cheilitis or nutritional deficiency. The results can guide the selection of antifungal agents or other treatments tailored to the specific type of infection identified.
Ultimately, the combination of clinical evaluation and laboratory tests provides a comprehensive view of the condition, leading to effective management of denture stomatitis for patients with removable dentures.
Common Laboratory Tests for Denture Stomatitis Diagnosis
| Test Type | Purpose |
|---|---|
| Swab cultures | To identify fungal organisms |
| Cytological smears | To determine the type of infection and fungal hyphae |
| Biopsy (if necessary) | To exclude other conditions |
List of Clinical Evaluation Aspects
- Visual inspection of the oral mucosa
- Assessment of denture fit and cleanliness
- Inquiry into symptoms such as sore mouth and discomfort
- Evaluation of oral hygiene habits and denture maintenance routine
- Duration of daily denture wear and overnight use
Denture wearers undergoing evaluation for suspected Denture Stomatitis should always follow the advice of dental professionals for the best outcomes in the treatment of their condition.
Treatment Options for Denture Stomatitis
Denture stomatitis is a treatable condition, and a multifaceted approach is often the most effective. Treatment aims to reduce inflammation, eliminate infection, and address any contributing factors to prevent recurrence. Below we’ll explore the different treatment options available for Denture Stomatitis.
Antifungal Medications
A primary method for treating the yeast infections associated with denture-related stomatitis is the use of antifungal medications. These can come in various forms, such as topical antifungal creams, oral lozenges, or systemic tablets.
Nystatin and clotrimazole are commonly prescribed antifungals for this condition. Denture wearers might be instructed to apply these agents directly onto the denture surface or the affected oral mucosal areas. In some cases, particularly when denture stomatitis is resistant to initial treatments, systemic antifungal medications like fluconazole may be necessary.
Proper Denture Care and Hygiene
Maintaining excellent denture hygiene is crucial in the treatment and prevention of denture stomatitis. Removable dentures should be thoroughly cleaned daily to remove food particles and microorganisms. This includes brushing them with a soft-bristled brush and non-abrasive cleanser, as well as soaking in a denture-cleansing solution. In addition, patients should remove their dentures at night to allow the oral mucosa to recover, reducing the risk of inflammation and infection.
Lifestyle Modifications
Changes in lifestyle can significantly impact the management of denture stomatitis. Smoking cessation is advised as smoking can exacerbate mucosal inflammation and disrupt the healing process. Additionally, a balanced diet rich in vitamins can help maintain healthy oral tissues, potentially minimizing the risk of inflammation. Limiting sugar intake can also discourage yeast growth in the oral cavity.
Regular Dental Checkups
Consistent follow-ups with a dental professional are critical for individuals managing denture stomatitis. Dental professionals can monitor the progress of treatment, adjust dentures for a better fit, and provide ongoing advice for effective oral hygiene practices.
Regular check-ups facilitate the early detection of any signs of relapse or complications, thereby allowing for prompt intervention. Patients should aim to visit their dentist at least once a year, or more frequently if recommended.
Prevention Strategies for Denture Stomatitis
Denture stomatitis is a common condition affecting the oral mucosa of individuals who wear complete or partial dentures. It is often associated with fungal infections, such as those caused by Candida species, poor denture hygiene, and ill-fitting dentures.
The condition is characterized by inflammation of the oral mucosa beneath the denture, which if left untreated, can lead to soreness and discomfort. Here are effective prevention strategies to mitigate the risk of developing denture stomatitis:
Nightly Denture Removal
To minimize the risk of developing denture-related stomatitis, one of the most important and simple preventive measures is the nightly removal of dentures. This practice helps reduce the accumulation of microorganisms and gives the palatal mucosa time to recover from the constant pressure and possible micro-traumas caused by denture wear. Furthermore, it decreases the closed, moist environment in which Candida thrives, helping to prevent fungal overgrowth.
| What | Why |
|---|---|
| Nightly denture removal | Allows oral tissues to rest and reduces microbial accumulation |
Maintaining Overall Oral Health
Denture wearers should not neglect their overall oral health. This involves maintaining the health of both the remaining natural teeth, if present, and the rest of the oral cavity. Attention should be paid to regular brushing of any natural teeth, cleaning of the gums, and the use of antifungal agents if needed.
It’s also important to ensure nutritional adequacy to support oral health and immune function. Regular dental checkups are crucial as they allow for the evaluation of denture fit and condition, as well as the timely management of any signs of oral conditions like denture stomatitis or angular cheilitis.
These preventative strategies aim to reduce the prevalence of denture stomatitis in denture wearers, ensuring comfort and overall oral health.
Thorough Cleaning Techniques
Denture stomatitis, commonly known as denture-related stomatitis or sore mouth, is a prevalent condition affecting the oral mucosa of denture wearers. This condition is often associated with poor denture hygiene, ill-fitting dentures, and the presence of yeast infections, especially those caused by Candida species. Proper oral hygiene is paramount for the prevention and management of denture stomatitis.
Thorough Cleaning Techniques for Denture Wearers:
- Remove and rinse dentures after eating to eliminate food particles.
- Clean the mouth after denture removal, focusing on gums, palate, and tongue.
- Brush dentures daily using a soft-bristle brush and nonabrasive cleanser.
- Soak dentures in a denture-cleansing solution as recommended by dental professionals.
- Rinse dentures thoroughly before putting them back in the mouth.
It’s crucial to maintain regular check-ups with dental professionals to ensure dentures fit properly and to receive guidance on the best cleaning practices. Additionally, replacement of worn or ill-fitting dentures can help prevent the development of denture stomatitis. Remember, while good denture care is necessary, it should always be accompanied by overall good oral hygiene practices.
Maintaining Overall Oral Health
Maintaining overall oral health is crucial for both general well-being and the prevention of oral conditions like denture stomatitis, a common condition among denture wearers. Here are key practices to follow for good oral hygiene:
Good Oral Hygiene Practices:
- Brush and Floss Regularly: Brush at least twice a day and floss once to remove plaque and food particles.
- Clean Dentures Daily: If you wear complete or partial dentures, clean them every day to prevent the buildup of food and bacteria.
- Rinse with Antiseptic Mouthwash: This can reduce the bacteria in the oral cavity.
Importance of Proper Denture Fit:
- Avoid Ill-Fitting Dentures: Ill-fitting dentures can cause a sore mouth and exacerbate conditions like denture-induced stomatitis.
Regular Dental Check-Ups:
- Consult Dental Professionals: Regular check-ups can help in the early detection and management of denture stomatitis.
Nutritional Considerations:
- Maintain a Balanced Diet: Nutritional deficiency can affect oral mucosa health.
Managing Denture Stomatitis:
- Seek antifungal treatment if symptoms of denture stomatitis, such as redness or discomfort in the palatal mucosa, occur.
In conclusion, good oral hygiene, proper denture care, and regular dental visits are essential in maintaining oral health and preventing denture-related conditions.
Psychological Impact of Denture Stomatitis
Denture stomatitis, commonly referred to as denture-related stomatitis, is a condition impacting the oral mucosa of individuals who wear full or partial dentures. While its physical symptoms are widely acknowledged, the psychological impact cannot be understated.
Individuals suffering from denture stomatitis often experience a sore mouth, which can lead to difficulties in eating, speaking, and socializing, culminating in a decreased quality of life. This discomfort can prompt self-consciousness and social withdrawal due to the altered appearance and fear of a noticeable oral malodor, further exacerbating feelings of embarrassment and isolation.
The worry of persistent health issues, as well as the burden of managing consistent oral hygiene and potential medical treatments, can also contribute to increased stress levels. The condition may severely impact the elderly, as they are more prone to wearing complete dentures. Such psychological strains can hinder overall well-being, emphasizing the importance of thorough education and support from dental professionals in the management of denture stomatitis.
For those affected by this common condition, understanding and addressing the psychological ramifications are just as important as treating its physical manifestations.
When to Consult a Dentist
Consulting a dental professional is crucial in the proactive management of denture stomatitis. Patients with denture stomatitis should not hesitate to reach out to their dentist if they experience persistent or concerning symptoms.
Furthermore, routine dental check-ups can help prevent the occurrence or the worsening of denture-related conditions. Individuals should seek dental advice if they notice any discomfort, particularly if they are new denture wearers or have recently had a denture fitting.
Warning Signs to Look Out For
Denture wearers should be attentive to any changes within their oral cavity to identify potential symptoms of denture stomatitis early. Here are warning signs that indicate the need for a consultation with a dental professional:
- Redness and Swelling: Visible redness or swelling of the oral mucosa, especially under the upper denture, is a common sign.
- Soreness and Pain: An unexplained or persistent sore mouth or gum pain should be addressed by a dentist.
- Raised Red or White Patches: The presence of raised lesions or white patches on the palatal mucosa may indicate yeast infection or other oral conditions.
- Bleeding: If the gums or oral tissues bleed when the dentures are removed or while cleaning.
Common Symptoms of Denture Stomatitis
| Symptom | Description | Area of Concern |
|---|---|---|
| Redness | Generalized or localized redness under the denture base | Palatal mucosa |
| Swelling | Puffiness or inflammation that can be gentle to the touch | Oral mucosa |
| Soreness and Pain | Discomfort or pain, which may be constant or during use | Oral mucosa/Gum line |
| White Patches | Whitish lesions or spots indicating possible yeast presence | Palatal mucosa |
| Bleeding | Uncommon but notable sign warranting prompt attention | Oral tissues/Gum line |
For individuals displaying these symptoms, scheduling an appointment with their dentist is imperative. Addressing and treating denture stomatitis early can prevent further complications, reduce discomfort, and maintain oral health.
Dental professionals will identify the underlying cause, which could range from poor denture hygiene to nutritional deficiency and will prescribe the appropriate course of treatment, such as antifungal agents or adjustments to the fit of the dentures.
FAQs
What is the recovery time for denture stomatitis?
The recovery time for denture stomatitis can vary, depending on the severity of the condition and how quickly treatment is started. With proper management, including antifungal treatment and improved denture care, symptoms may begin to improve within a few days.
However, it can take several weeks for the mucosa to fully heal and for the comfort with the dentures to be re-established. Regular follow-ups with dental professionals are important in ensuring a timely recovery, and patients should adhere closely to the treatment regimen prescribed.
Can denture stomatitis recur after treatment?
Yes, denture stomatitis can recur after treatment. This recurrence is often due to the same factors that contributed to its initial development, such as ill-fitting dentures, poor oral hygiene, and chronic yeast infections.
To minimize the risk of recurrence, patients are advised to maintain consistent and thorough oral hygiene, ensure that their dentures fit properly, and have regular dental check-ups. Sometimes, even after addressing these factors, reinfection can happen, requiring additional treatment.
How can I maintain oral hygiene with dentures?
Maintaining oral hygiene with dentures is crucial to preventing denture stomatitis and other oral health issues. Below is a list of recommendations:
- Clean Dentures Daily: Remove and gently clean your dentures each day using a soft-bristle toothbrush and a nonabrasive denture cleaner.
- Soak Dentures: Soak dentures in a cleansing solution overnight, or as directed by your dental professional, to help kill bacteria and fungi.
- Brush Gums, Tongue, and Palate: Before inserting dentures, brush your gums, tongue, and palate with a soft-bristle brush to remove plaque and stimulate circulation.
- Rinse After Eating: Rinse your mouth with water after meals to remove food particles and debris.
- Visit the Dentist Regularly: Regular dental visits are essential for professional cleaning and checking the fit of your dentures.
- Avoid Abrasive Cleaning Materials: Harsh cleansers or stiff brushes can damage dentures.
- Keep Dentures Dry when not in Use: This can help prevent the growth of yeast and other microorganisms.
By following these guidelines for oral hygiene and denture care, you can help maintain a healthy oral environment and reduce the risk of developing denture-related complications.
What is the recovery time for denture stomatitis?
| Factor Affecting Recovery | Estimated Recovery Time |
|---|---|
| Antifungal Treatment | 2-4 weeks |
| Denture Adjustment | Varies |
| Improved Oral Hygiene | Varies |
| Nutritional Intervention | Varies |
| Combined Conditions | May extend beyond 4 weeks |





